Methods
Summary
STUDY AIM
This study intends to determine feasibility of a music therapy protocol as intervention to support respiration, cough, swallowing and speech functions of persons with amyotrophic lateral sclerosis. Since music therapy constitutes a new treatment modality for bulbar and respiratory dysfunction in ALS, the study is focused primarily on safety and tolerability of the treatment protocol.
Applied music therapy research in multidisciplinary clinical context allows to systematically look at bulbar and respiratory functions support in ALS, which is important to do, since swallowing, vocalization and breathing are tightly coordinated, and close relationship exists between these processes, in terms of location and activation of the neurons (Larson, Yajima et al., 1994), (Matsuo, 2008).
RESEARCH QUESTIONS
Primary:
Do music therapy exercises slow down the decline of respiratory and bulbar functions in patients with early and mid-stage ALS?
Secondary:
- Which are the most effective standard tools that can be used to measure the effect of music therapy protocol on respiratory and bulbar functions of ALS patients?
- How feasible are the experimental conditions (in terms of safety and tolerability of the suggested music therapy protocol, adherence to treatment, adherence to data collection)?
STUDY DESIGN
The study employs single-case research design: each participant will receive treatment and will serve as his / her own control. The duration of participation in the study will be sixteen weeks, including lead-in phase (weeks 1 through 6), treatment phase (weeks 7 through 12) and wash out phase (week 13 through 16).
MUSIC THERAPY TREATMENT PROTOCOL
Upper motor neurons and lower motor neurons deterioration in ALS results in dysarthria and dysphagia of spastic-flaccid type, although actual presentation varies in each patient and changes with the disease progression. Generally, lower motor neurone (LMN) involvement, characteristic of bulbar onset, leads to flaccid presentation, whilst degeneration of upper motor neurone (UMN), characteristic of spinal onset, results in spasticity of bulbar muscles. Muscle relaxation and moderate exercise, as well as learning efficient breathing and voice production techniques, voice care techniques and ALS-specific communication strategies may be helpful, rather than rigorous strengthening oral motor exercises. The protocol serves the following primary therapy objectives:
- to increase breath support,
- to increase muscle relaxation,
- to increase speech rate,
- to prevent / decrease hypernasality,
- to maintain swallowing coordination.
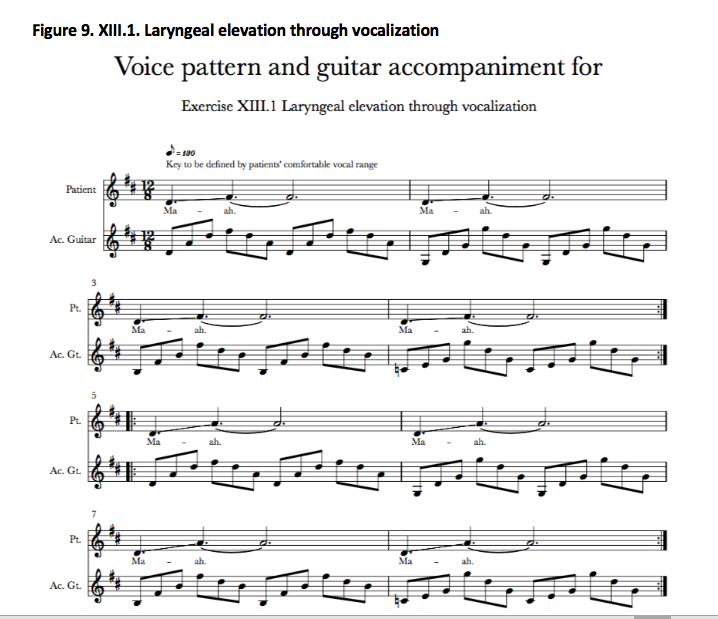
ALS-specific, individualized MT protocol was delivered to study participants in their homes twice weekly for the duration of six weeks by the researcher, who is a board certified music therapist and neurologic music therapist, with experience of working with this patient group and in this setting. Facilitating music structures were composed by the researcher to support cueing, timing and intensity of breathing and vocalization exercises. These structures were regularly modified to suit the unique capabilities, current individual demands and progress of each participant. Individualized sets of music therapy exercises were recorded (and updated as needed) for each participant for independent everyday practice:
IMPORTANT NOTE
This is the first music therapy treatment protocol for rehabilitation of respiratory and bulbar functions of persons with ALS / MND. We believe that, for safety of persons with ALS / MND, it is not ethically sound to share the treatment protocol whilst the research is still underway. Full music therapy treatment protocol, with the necessary adjustments and commentaries, will be made public as a result of this study at http://alsmusictherapy.org before 2020.
Challenges
GENERAL CHALLENGES
Research on clinical music therapy applications for ALS is insufficient (Horne-Thompson & Grocke, 2010) and presents significant challenges for a researcher due to heterogeneity of ALS clinical presentation and progression, poor scientific understanding of the disease mechanisms (Bonafede & Mariotti, 2017) and the ethical issues of research involving people in palliative care (Byock, 2003).
THE ROLE OF EXERCISE IN ALS
Prior to recently the exercise has been discouraged for people with ALS, the recommendation based on the assumption that exercise can lead to muscle fatigue and, hence, to increase patient’s disability (Sinaki & Mulder, 1978). Recent data suggests that exercise may be beneficial for cellular and morphological adaptations in motor neuron function and thus may help to maintain motor function (Plowman et al, 2015). Finally, (Lunetta et al., 2016) preliminary RCT results suggest that strictly monitored exercise programs reduce motor deterioration in ALS. Thus, in current clinical practice regular moderate exercise is encouraged for people with ALS to prolong mobility and independence.
Even more so than in case of the general physical exercise, there is lasting controversy in regards to the role of exercise in management of bulbar and respiratory ALS symptoms. Emerging evidence suggests that respiratory training may have positive effect on respiratory and swallowing functions of people with ALS (Pinto, Swash and de Carvalho, 2012), (Plowman et al., 2016), (Tabor et al, 2016). There is obvious need for continued research and higher levels of evidence to understand the role of exercise in bulbar and respiratory rehabilitation in ALS (Hanson, Yorkston & Britton, 2011), (Plowman, 2015).
Since music therapy constitutes a new treatment modality for bulbar and respiratory dysfunction in ALS, the study is focused primarily on safety and tolerability of the treatment protocol. Our protocol was designed to allow for ample rest and relaxation possibilities between short exercises involving active muscle work, in order to prevent fatigue. The exercises were skipped or modified if the patient felt uncomfortable or tired, or if the exercise did not meet the patient’s actual clinical needs.
DEFINING APPROPRIATE MEASUREMENT TOOLS
Choosing the effective tools to measure the effect of music therapy protocol on respiratory and bulbar functions of people with ALS has been arguably the most challenging part of this research so far. “No standardized diagnostic procedure for assessing bulbar dysfunction in ALS exists and adequate objective markers of bulbar deterioration have not been identified”, thus “clinicians invariably find it challenging to predict the rate of speech and swallowing decline” (Green et al., 2013)
Following the analysis of existing research, including (Baker et al, 2005), (Tamplin, 2008), (Nishio and Niimi, 2000), (Strand et al., 1994), (Bowen, 2013), (Plowman, 2015), (Rong et al., 2016), (Andersen et al., 2005), (Pinto, 2017), (Yunusova et al., 2011), (Beukelman et al., 2011), (Lee, 2017), (Mefferd et al., 2012), (Pinto, 2017), (Wiens et al., 1999), (Czaplinski et al., 2006), (Yunusova et al., 2011), (Haneishi, 2001), (McCullough et al., 2012), (Mendelsohn, 1987), (Touré‐Tillery and Fishbach, 2014), (Brédart et al., 2014), (Pietkiewicz & Smith, 2014), (Donovan et al., 2008) and professional consultations with some of the authors and with ALS clinical care practitioners, we have decided upon the measurement tools that are listed below (see “Data analysis” section).
Pre Analysis Plan
DATA ANALYSIS is being completed with help of a qualified statistician at Anglia Ruskin University in order to:
- understand the individual long-term effect of the music therapy treatment on bulbar and respiratory dysfunction of the participants with ALS;
- understand the individual short-term effect of the music therapy treatment on bulbar and respiratory dysfunction of the participants with ALS;
- understand the mean long-term effect of the music therapy treatment on bulbar and respiratory dysfunction of the participants with ALS for the whole group;
- understand the mean short-term effect of the music therapy treatment on bulbar and respiratory dysfunction of the participants with ALS for the whole group;
- assess feasibility of the suggested music therapy protocol for treatment on bulbar and respiratory dysfunction of the participants with ALS, in terms of safety, tolerability and adherence for the patients;
- assess feasibility of the suggested regimen for home-based music therapy treatment on bulbar and respiratory dysfunction of the participants with ALS, in terms of treatment coordination, therapist travel and work, suitability of home environment for treatment, etc;
- assess feasibility of the research protocol implementation, including recruitment pool and recruitment rate, study design, data collection, sensitivity of the selected measurement tools to changes;
- assess feedback from research participants regarding their music therapy experiences.
The PRIMARY OUTCOME MEASURES include:
- Change of Forced Vital Capacity (FVC) from baseline at Week 6, Week 12, Week 16
- Change of Maximal Inspiratory Pressure (MIP) from baseline at Week 6, Week 12, Week 16
- Change of Maximal Expiratory Pressure (MEP) from baseline at Week 6, Week 12, Week 16
- Change of Peak Cough Flow (PCF) from baseline at Week 6, Week 12, Week 16
- Change of Center for Neurologic Study Bulbar Function Scale (CNS-BFS) Swallowing subscore from baseline at Week 6, Week 12, Week 16
- Change of Center for Neurologic Study Bulbar Function Scale (CNS-BFS) Speech subscore from baseline at Week 6, Week 12, Week 16
- Change in video fluoroscopic swallowing study (VFSS) results from baseline at Week 6, Week 12
- Change in acoustic assessment parameters of recorded voice from baseline at Week 6, Week 12, Week 16
- Change in Visual Analogue Scale for current perceived ease of respiration from pre-treatment to post-treatment
- Change of Visual Analogue Scale for current perceived ease of speech from pre-treatment to post-treatment
- Phenomenological analysis of participant semi-structured interviews pre-treatment
- Phenomenological analysis of caregiver semi-structured interview pre-treatment
- Phenomenological analysis of treatment sessions documentation
- Phenomenological analysis of participant semi-structured interviews post-treatment
- Phenomenological analysis of caregiver semi-structured interview post-treatment
Analysis of variance (ANOVA), t-test and paired t-test procedures are being used to analyze objective data, as well as interpretative phenomenological analysis (for semi-structured interviews and participant’s statements in reflections during music therapy sessions) and descriptive analysis (case studies).
Protocols
Browse the protocols that are part of the experimental methods.