Please wait...
About This Project
OncoSynergy, Inc.
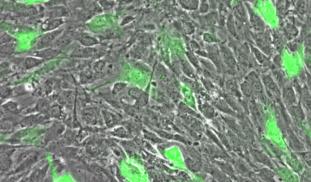
The Ebola outbreak in west Africa has been declared a global emergency by the WHO with over 1,000 victims and no approved therapies. OncoSynergy is developing a readily manufactured experimental cancer drug, OS2966, which coincidentally targets the receptor hijacked by ebola to infect cells. This project aims to demonstrate that OS2966 inhibits ebola infection of human cells thus providing the impetus for expediting OS2966 for treatment of ebola.

Browse Other Projects on Experiment
Related Projects
CaniSense– AI-powered blood test for early cancer detection in dogs
Cancer is the top killer of dogs, yet no reliable early screening exists. We develop liquid-biopsy blood...
Shutting down cancer’s recycling system with exosome-based therapy
Pancreatic cancer is one of the deadliest cancers because its cells survive by recycling their own components...
Developing a novel oxysterol antibiotic to combat drug-resistant tuberculosis
Drug-resistant tuberculosis (TB) is a consistently growing threat to global health. We have developed Oxy291...