Music Therapy Protocol to Support Bulbar and Respiratory Functions in ALS
Brief Summary:
This study evaluates potential of music therapy treatment to support breathing, speech, swallow and cough of persons with amyotrophic lateral sclerosis (ALS). Music therapy is the clinical use of music and its elements to enhance human health and wellbeing. Application of music therapy principles in neurorehabilitation allow to treat cognitive, sensory, and motor dysfunctions.
Study Type : Interventional (Clinical Trial)
Actual Enrollment : 8 participants
Intervention Model: Single Group Assignment
Intervention Model Description: Single-subject design (Repeated measures)
Masking: None (Open Label)
Primary Purpose: Health Services Research
Official Title: Measuring the Effects of a Music Therapy Protocol on Respiratory and Bulbar Functions of Patients With Early and Mid-stage Amyotrophic Lateral Sclerosis: Mixed Methods Single Case Study Series
Actual Study Start Date : September 27, 2017
Estimated Primary Completion Date : July 31, 2018
Estimated Study Completion Date : January 1, 2020
Study aim
This study intends to determine feasibility of a music therapy protocol as intervention to support respiration, cough, swallowing and speech functions of persons with amyotrophic lateral sclerosis. Since music therapy constitutes a new treatment modality for bulbar and respiratory dysfunction in ALS, the study is focused primarily on safety and tolerability of the treatment protocol.
Applied music therapy research in multidisciplinary clinical context allows to systematically look at bulbar and respiratory functions support in ALS, which is important to do, since swallowing, vocalization and breathing are tightly coordinated, and close relationship exists between these processes, in terms of location and activation of the neurons (Larson, Yajima et al., 1994), (Matsuo, 2008).
Research questions
Primary:
Do music therapy exercises slow down the decline of respiratory and bulbar functions in patients with early and mid-stage ALS?
Secondary:
- Which are the most effective standard tools that can be used to measure the effect of music therapy protocol on respiratory and bulbar functions of ALS patients?
- How feasible are the experimental conditions (in terms of safety and tolerability of the suggested music therapy protocol, adherence to treatment, adherence to data collection)?
Study design
The study employs single-case research design: each participant will receive treatment and will serve as his / her own control. The duration of participation in the study will be sixteen weeks, including lead-in phase (weeks 1 through 6), treatment phase (weeks 7 through 12) and wash out phase (week 13 through 16).
Experimental Arm: Music therapy protocol
Each participant received 12 home-based music therapy treatment sessions over 6-week time period.
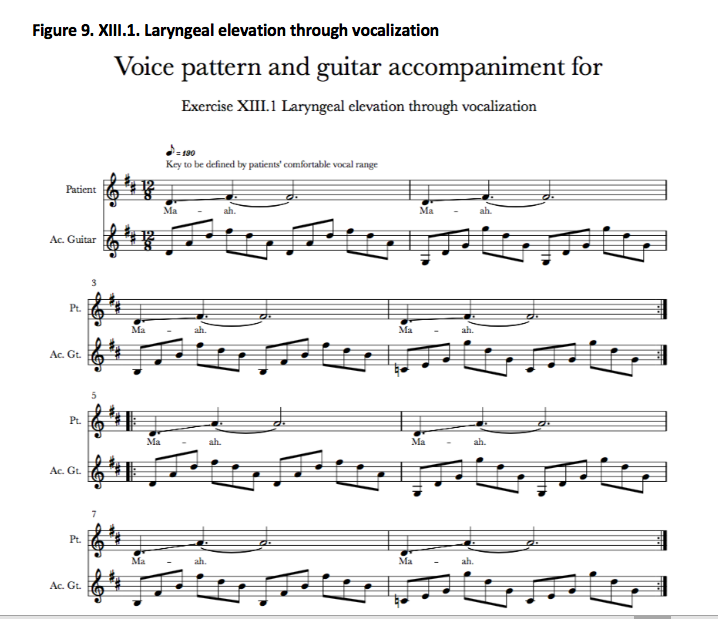
Procedure: Music therapy ALS-specific, individualized MT protocol was delivered to study participants in their homes twice weekly for the duration of six weeks by the researcher. Facilitating music structures were composed by the researcher to support cueing, timing and intensity of breathing and vocalization exercises. These structures were regularly modified to suit the unique capabilities, current individual demands and progress of each participant. One familiar song, selected by the participant, was used for each participant in therapeutic singing exercise closing each session. Individualized exercises sets for independent practice were provided at session 3 to each participants. ALS-specific voice health guidelines were provided for participants prior to start of the treatment.
Music therapy treatment protocol
Upper motor neurons and lower motor neurons deterioration in ALS results in dysarthria and dysphagia of spastic-flaccid type, although actual presentation varies in each patient and changes with the disease progression. Generally, lower motor neurone (LMN) involvement, characteristic of bulbar onset, leads to flaccid presentation, whilst degeneration of upper motor neurone (UMN), characteristic of spinal onset, results in spasticity of bulbar muscles. Muscle relaxation and moderate exercise, as well as learning efficient breathing and voice production techniques, voice care techniques and ALS-specific communication strategies may be helpful, rather than rigorous strengthening oral motor exercises. The protocol serves the following primary therapy objectives:
to increase breath support,
to increase muscle relaxation,
to increase speech rate,
to prevent / decrease hypernasality,
to maintain swallowing coordination.
ALS-specific, individualized MT protocol was delivered to study participants in their homes twice weekly for the duration of six weeks by the researcher, who is a board certified music therapist and neurologic music therapist, with experience of working with this patient group and in this setting. Facilitating music structures were composed by the researcher to support cueing, timing and intensity of breathing and vocalization exercises. These structures were regularly modified to suit the unique capabilities, current individual demands and progress of each participant. Individualized sets of music therapy exercises were recorded (and updated as needed) for each participant for independent everyday practice.
IMPORTANT NOTE
This is the first music therapy treatment protocol for rehabilitation of respiratory and bulbar functions of persons with ALS / MND. We believe that, for safety of persons with ALS / MND, it is not ethically sound to share the treatment protocol whilst the research is still underway. Full music therapy treatment protocol, with the necessary adjustments and commentaries, will be made public as a result of this study at http://alsmusictherapy.org before 2020.
Inclusion Criteria:
· Newly diagnosed patients at ALS Centre Moscow (consecutive sampling)
· Diagnosis of probable or definite ALS by the revised El Escorial criteria confirmed by neurologist at ALS Moscow Centre prior to screening for enrollment.
· Amyotrophic Lateral Sclerosis Functional Rating Scale - Revised (ALSFRS-R) bulbar subscore ≥ 9, but ≤ 11, where bulbar score=the sum of ALSFRS-R questions 1-3 (maximum score of 12)
· Forced vital capacity (FVC) greater than 60%
· Unimpaired cognition as evidenced by Edinburgh Cognitive and Behavioural ALS Screen (ECAS) cut-off scores adjusted for age and education
· Able to consent to treatment
· Native speakers of Russian
Exclusion Criteria:
· Tracheostomy or mechanical ventilation
· Diaphragmatic pacer
· Significant concurrent respiratory disease
· Allergies to barium
· Receiving any other experimental treatment for dysarthria, dysphagia, dystussia and dyspnoea for the duration of the study
· Receiving any other music therapy treatment for the duration of the study
Primary Outcome Measures:
- Change of Forced Vital Capacity (FVC) from baseline at Week 6, Week 12, Week 16 [ Time Frame: Throughout the field phase of the study (16 weeks) ]FVC is a standard spirometry test which measures the volume of air that can forcibly be blown out after full inspiration.
- Change of Maximal Inspiratory Pressure (MIP) from baseline at Week 6, Week 12, Week 16 [ Time Frame: Throughout the field phase of the study (16 weeks) ]MIP is the inspiratory pressure generated against a completely occluded airway; used to evaluate inspiratory respiratory muscle strength.
- Change of Maximal Expiratory Pressure (MEP) from baseline at Week 6, Week 12, Week 16 [ Time Frame: Throughout the field phase of the study (16 weeks) ]MIP is a measure of the strength of respiratory muscles, obtained by having the patient exhale as strongly as possible against a mouthpiece.
- Change of Peak Cough Flow (PCF) from baseline at Week 6, Week 12, Week 16 [ Time Frame: Throughout the field phase of the study (16 weeks) ]PCF is a measure of cough effectiveness, portable peak flow meter was used.
- Change of Center for Neurologic Study Bulbar Function Scale (CNS-BFS) Swallowing subscore from baseline at Week 6, Week 12, Week 16 [ Time Frame: Throughout the field phase of the study (16 weeks) ]The Center for Neurologic Study Bulbar Function Scale (CNS-BFS) consists of three domains (swallowing, speech, and salivation), each of which is assessed with a 7-item, self report questionnaire. Each question is scored from "1" (does not apply) to "5" (applies most of the time). Swallowing domain subscore can range from "7" (best outcome) to "35" (worst outcome).
- Change of Center for Neurologic Study Bulbar Function Scale (CNS-BFS) Speech subscore from baseline at Week 6, Week 12, Week 16 [ Time Frame: Throughout the field phase of the study (16 weeks) ]The Center for Neurologic Study Bulbar Function Scale (CNS-BFS) consists of three domains (swallowing, speech, and salivation), each of which is assessed with a 7-item, self report questionnaire. Each question is scored from "1" (does not apply) to "5" (applies most of the time). Speech domain subscore can range from "7" (best outcome) to "35" (worst outcome).
- Change in video fluoroscopic swallowing study (VFSS) results from baseline at Week 6, Week 12 [ Time Frame: Throughout the field phase of the study (16 weeks) ]VFSS is an x-ray-based method of evaluating a person's swallowing ability.
- Change in acoustic assessment parameters of recorded voice from baseline at Week 6, Week 12, Week 16 [ Time Frame: Throughout the field phase of the study (16 weeks) ]Machine-analyzed set of structured voice samples.
- Change in Visual Analogue Scale for current perceived ease of respiration from pre-treatment to post-treatment [ Time Frame: Throughout the therapy phase (6 weeks) ]Visual Analogue Scale (VAS) for current perceived ease of respiration is a one question 10-point scale administered at the beginning and at the end of every music therapy session to assess short-term change in current perceived ease of respiration. The outcome can range from "1" (very difficult) to "10" (very easy).
- Change of Visual Analogue Scale for current perceived ease of speech from pre-treatment to post-treatment [ Time Frame: Throughout the therapy phase (6 weeks) ]Visual Analogue Scale (VAS) for current perceived ease of speech is a one question 10-point scale administered at the beginning and at the end of every music therapy session to assess short-term change in current perceived ease of speech. The outcome can range from "1" (very difficult) to "10" (very easy).
- Phenomenological analysis of participant semi-structured interviews pre-treatment [ Time Frame: Week 5 ]Analysis of participant's answers to open questions in regards to expectations for music therapy treatment
- Phenomenological analysis of caregiver semi-structured interview pre-treatment [ Time Frame: Week 5 ]Analysis of main caregiver's answers to open questions in regards to expectations for music therapy treatment
- Phenomenological analysis of treatment sessions documentation [ Time Frame: Throughout the therapy phase (6 weeks) ]Analysis of narrative accounts of music therapy sessions submitted by the therapist
- Phenomenological analysis of participant semi-structured interviews post-treatment [ Time Frame: Week 13 ]Analysis of participant's answers to open questions in regards to impressions of music therapy treatment
- Phenomenological analysis of caregiver semi-structured interview post-treatment [ Time Frame: Week 13 ]Analysis of main caregiver's answers to open questions in regards to impressions of music therapy treatment
- Published on Nov 20, 2018
- 99 views
- 0 comments
- Print this page
- Back to Methods